Awards
Throughout the year, the College of Anaesthesiologists of Ireland, administers a number of distinguished award schemes and prizes. The College conducts many research and scholarship competitions that provide doctors with opportunities to gain funding and to publish research. We are updating the list of beneficiaries of awards, from previous years, and welcome information on previous winners.
In 2018 the College launched a new award to recognise excellence in training by our trainer doctors. Dr Sheila O’ Callaghan, Consultant Anaesthetist in Cork University Hospital and Dr Patricija Ecimovic, Consultant Anaesthetist in University Hospital Waterford were recognised as being excellent mentors by their trainees, in a national poll of doctors in training to become specialist anaesthestists. Each year, trainee doctors affiliated with the College of Anaesthesiologists of Ireland who undergo training in hospitals across Ireland vote on the best consultants in terms of training provided.
Recent Winners:
- 2024: Dr Michelle Duggan and Dr Joathan Roddy
This lecture is integrated into the annual Core Topics Day meeting which is held in October. The presenter of this lecture is awarded the Autumn College Lecture medal in recognition of their work.
Previous Winners
- 2015: Dr Fionnuala Ni Ainle, Mater Misericordiae University Hospital, Dublin. ‘Obstetric Haemorrhage’.
- 2014: Professor Robert Sneyd,Dean of the Plymouth University Peninsula Schools of Medicine and Dentistry, UK. “Time to change our practice?”
- 2013: Dr Stephen Prineas, Guy’s Hospital and Imperial College Healthcare NHS Trust. “Blazing a Vapour Trail – Why Anaesthetists Can and Should Take the Lead on Human Factors Training”
- 2012: Dr Brendan McGrath, Manchester. “Another difficult airway: The UK National Tracheostomy Safety Project”
- 2011: Prof Mike James, Head of Department of Anaesthesia, University of Cape Town and Groote Schuur Hospital. ‘Core issues with anaesthesia for thyroids’.
- 2010: Prof Rajinder Mirakhur, Belfast. This presentation was entitled ‘From poisoned arrows to safe sugars”
- 2009: Prof Brendan Madden
- 2008: Dr Michael McBrien
- 2007: Prof Pierre Coriat ‘The Effects of Cardiovascular Treatment Regimens on Patient Outcome following major vascular surgery’
- 2006: Prof Philip Routledge ‘Herbal Medicines and the Anaesthetists’
- 2005: Prof John Henry ‘Too hot to handle’
- 2004: Dr Jack McCluggage
Brian Kavanagh Brian Kavanagh graduated from University College Dublin in 1985, winning the Maginnis gold medal for Medicine at St Vincent’s University Hospital. He obtained his Medical Membership of the Royal College of Physicians in 1988. He completed training in Anesthesiology at the University of Toronto, receiving his Fellowship of the Royal College of Physicians and Surgeons of Canada in 1992. Following residency training in Toronto, Brian completed clinical and research fellowship training in critical care at Stanford University. Brian returned to Toronto in 1994, appointed as staff anesthesiologist and intensivist at the Toronto General Hospital, where he founded his research laboratory. In 1999, Brian was recruited to the Hospital for Sick Children, where he received the Geoffrey Barker Chair in Critical Care Medicine in 2003. Brian was appointed the Chair of the Department of Anesthesia at the University of Toronto in 2006, and served two highly successful terms until 2017. Brian was an exemplary clinician-scientist and was a gifted educator and bedside teacher. He was adored by his patients and their families, and he was a brilliant, highly productive researcher whose work has benefitted countless patients and will continue to do so well into the future. Brian co-authored nearly 200 peer-reviewed research papers, many in the highest impact journals such as NEJM, Lancet, BMJ, and his laboratory was extremely successful in attracting peer-reviewed funding from grant agencies such as the Canadian Institutes for Health Research. Brian was elected a fellow of the Canadian Academy of Health Sciences in May 2012, an uncommon achievement in our field. He was awarded a highly prestigious Tier 1 Canada Research Chair by the Government of Canada, which is bestowed upon outstanding researchers acknowledged by their peers as world leaders in their fields. He was the first anesthesiologist to be so honoured. Irish and Canadian anesthesia and intensive care medicine lost a passionate and visionary leader when Brian Kavanagh passed away on June 15th, 2019, at the age of 57. This annual lecture rightly marks his legacy and contribution to Irish Anaesthesiology and Intensive Care Medicine.
Previous Presenters
- 2024: Dr John Boylan, ‘ICSI Lecture’
- 2021: Dr Martin J Tobin, ‘Consensus, controversy and medicine’
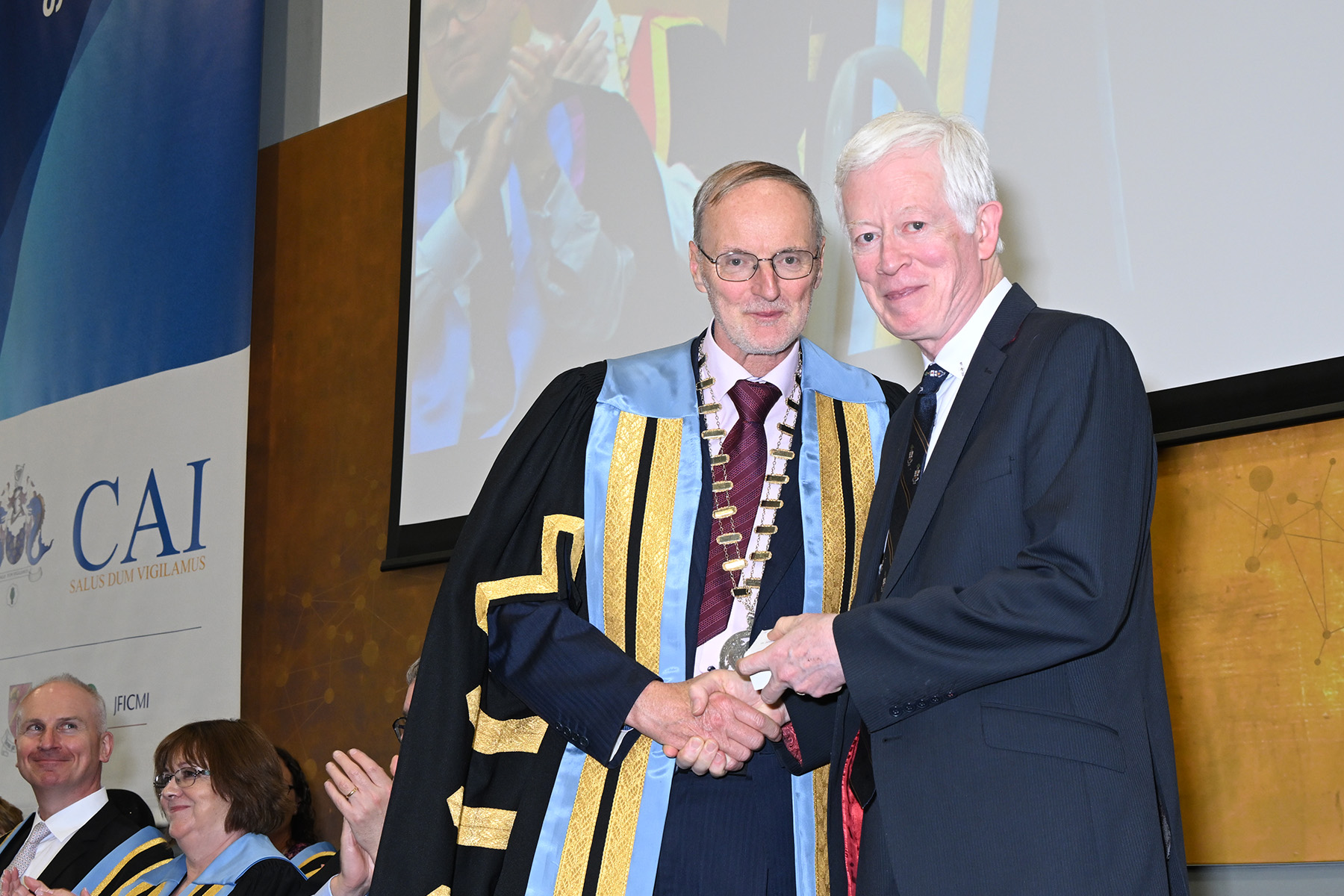
This is the highest award that the College can make. The President of the College along with College Council may consider eminent individuals for the award who have given outstanding service to the specialty of anaesthesiology, intensive care medicine and pain medicine over many years and are renowned internationally.
The award is not restricted to anaesthesiologists however, so that clinicians from other medical specialties, scientists working on non medical areas and leaders of industry whose work has advanced our understanding of anaesthesia and generally raised the profile of anaesthesia may be considered for Honorary Fellowship.
The award is made annually and usually there are no more than two to three recipients at a time. The formal ceremony takes place at one of the College’s major academic meetings during when a citation is read and later presented to the new Honorary Fellow as a memento of the occasion.
Honorary Fellows:
|
|
|
This medal is awarded to anaesthesiologists who have given outstanding service to the specialty of anaesthesiology and the College over many years by virtue of their commitment to teaching and training or by holding high office in the College, though not the Presidency.
Individuals who, over a shorter period of time, have raised the profile of the College nationally and internationally by undertaking major projects or endeavours that have far reaching significance for both clinicians and patients, may also be considered for the College medal.
The College medal is awarded by the President and Council in alternate years.
Recent Winners:
- 2024 Dr Maria Donnelly & Dr John Boylan
- 2020 Catherine Motherway
- 2020 Deirdre McCoy
- 2019 Cyril Goddia
- 2019 Tom Schnittger
- 2018 Alan McShane
- 2018 Mary Stritch
- 2017 Declan O’Brien
- 2017 Declan Warde
- 2017 Gerard Browne
- 2016 Roisin M MacSullivan
- 2016 John Cahill
- 2015 Ian Surgeon
- 2015 Wouter Jonker
- 2015 Billy Casey
- 2013 Tipu Sultan
- 2012 John Howe
- 2012 Carlos McDowell
- 2010 Seamus Hart
- 2009 Angela Enright
- 2008 Archibald Brain
The Membership Exam Medal is awarded to a candidate who on their first attempt at the Membership exam (formerly known as the Primary Fellowship) achieves an A grade in all sections of the examination. The medal is awarded at the annual conferring ceremony in May.
Recipients
- Spring 2024 Dr Cathriona Murphy
- Autumn 2023 Dr Aneeqa Tahir
- Spring 2021 Sean Boyd
- Autumn 2020 Gillian Crowe
- Autumn 2019 John O’Shea
- Spring 2019 Syed Ziad Ali
- Autumn 2018 Oscar Duffy
- Autumn 2017 Stephen Murphy
- Autumn 2017 Craig Lyons
- Autumn 2017 Eoin Kelleher
- Spring 2016 John O’Connor
- Autumn 2015 Aogan Ó Muircheartaigh
- Spring 2015 Grainne Rooney
- Autumn 2014 Ruairi Irwin
- Autumn 2014 Donogh Burns
- Autumn 2013 Anusha Kannan
- Autumn 2012 Bill Walsh
- Spring 2012 David Greaney
- Autumn 2011 Mary Aisling McMahon
- Spring 2010 Raymund O’Connor
- Spring 2009 Jacques Diacono
- Autumn 2007 Jennifer Hastings
- Spring 2006 Sibi Sebastian
- Autumn 2006 Niall Fanning
- Spring 2005 Chetana Kataria
- Autumn 2004 David Sommerfield
- Spring 2004 Subramanian Ramani
- Spring 2002 Raman Sivasankar
- Autumn 2002 Róisín Ní Mhuircheartaigh
- Spring 1996 Dara Breslin
- Autumn 2001 Donal Martin
- Spring 1995 Stephen Austin
- Spring 1991 Paul Loan
- Spring 1989 Brendan O’Hare
- Autumn 1984 Peter Randalls
- Autumn 1983 Raymond Allen
- Spring 1982 Pamela Bell
- Autumn 1982 Georgi Liting Sin Samsoon
- Spring 1981 Gavin Lavery
- Autumn 1981 Aidan Synnott
- Autumn 1978 Pamela Elizabeth MacIntyre
- Spring 1977 Vimala Parasuram Bhatt
- Autumn 1976 Enda Shanahan
- Spring 1976 Melvyn Fyffe Thomson
- Autumn 1975 Guranathan Pathy
- Autumn 1974 William O’Brien
- Autumn 1973 Claire Connolly
- Spring 1973 Richard John McBride
- Autumn 1971 Joan Neilson Lande
This medal commemorates the late Dr Edmund Delaney and is awarded by the Council of the College of Anaesthesiologists of Ireland to trainees for work carried out in Ireland on a subject related to anaesthetic practice. The Delaney Medal Competition winner is selected following two assessments; an abstract submission of their work and a presentation. Six abstracts are selected by three judges who then examine the applications. To maintain anonymity applicants must also submit under a ‘non de plume’ abstract form and a normal abstract form. Those selected to present at the Delaney Medal Competition are limited to 10 minutes. The judges may then ask questions for a further 5 minutes. The winner of the competition is announced that evening and is awarded the Delaney Medal. Applications are open from January and presentations are held in March annually. The competition is advertised by the Education Department (CAI), application information is available on the College website (www.anaesthesia.ie); all trainees are contacted directly and application information is distributed around all training hospitals. Edmund J Delaney 1925 – 1979 Edmund Delaney was born in Dublin and was the second youngest of four children. He was educated at Belvedere College and Clongowes Wood College and studied medicine at University College, Dublin. He graduated in 1949, MB, BCh, BAO and interned in the Mater Hospital. He immediately began training in anaesthesia firstly at Blackburn in Lancashire, then at the Norfolk & Norwich hospitals in East Anglia and finally as senior registrar at Dundee where he was also Tutor in anaesthesia at the University of St Andrews. Having gained the DA and the FFA RCS, Dr Delaney returned to Dublin in 1958 to take up a post as consultant anaesthetist at Dr. Steeven’s Hospital. He quickly gained a reputation as a dynamic and forward looking clinician and also as educator and teacher. He championed the use of neuraxial anaesthesia for both major hip surgery and gynaecological surgery and was also responsible for developing the anaesthetic expertise required for the care of infants and children undergoing repair of hair lip & cleft palate at the hospital, a fact which made Dr Steeven’s a much sought after slot on the anaesthesia training rotations which developed later. Edmund Delaney also played a major role in the establishment of the Faculty of Anaesthetists of the Royal College of Surgeons in Ireland, serving as a Board member (1965-1969 & 1974-1978) and as Vice Dean (1971-1973). He was a lecturer at Trinity College, Dublin, Chairman of the Anaesthetic section of the Irish Medical Association and Chairman of the Anaesthetic services of the Federated Dublin Hospitals. Edmund Delaney died at the peak if his career in 1979. In recognition of the outstanding contribution he had made to the specialty of anaesthesia in general and to the Faculty of Anaesthetists RCSI, in particular, the Board of Faculty instituted the Delaney Medal competition in 1981.
Previous Winners:
- 2024: Dr Nicole Naidoo
- 2021: Dr Oscar Duffy: ‘A National Audit of CO2 Equivalent Emissions from Inhalational Anaesthetic Gases’
- 2020: Dr Dylan Finnerty, ‘Prospective, Randomised, Double-Blind Clinical Trial comparing Erector Spinae Plane Block with Serratus Anterior Plane Block for Quality of Recovery and Morbidity after Minimally Invasive Thoracic Surgery’
- 2019: Dr Tom Wall, ‘Anaesthesia data in the era of machine learning’.
- 2018: Dr Jean-Francois Bonnet, ‘Safe reversal of neuromuscular blockade with low dose sugammadex. Is it time for smaller vials?’.
- 2017: Dr Thomas Drew, ‘Do supraglottic airways increase the accuracy of cricothyroid membrane identification in female patients? – a prospective observational study’.
- 2016: Dr Caroline Larkin, ‘Mechanisms of sepsis-induced platelet dysfunction’.
- 2015: Dr Karthikeyan Srinivasan ‘A comparison of conventional landmark guided midline versus pre-procedure ultrasound – guided paramedian techniques in spinal anesthesia’.
- 2014: Dr Stephen Frohlich ‘Human The CREB transcription factor mediates pulmonary hypoxic responses; implications for a novel therapeutic strategy in ARDS’.
- 2013: Dr Mairead Hayes ‘Human mesenchymal stem cells enhance repair following ventilator-induced lung injury’.
- 2012: Dr Gerard Curley, his presentation was entitled ‘The use of intra-tracheal Mesenchymal Stem Cells therapy to enhance repair of the injured lung’
- 2011: Dr Mary White, ‘Mesenchymal Infection and sepsis in humans is associated with deficient gene expression of γc cytokines’.
- 2010: Dr Tadhg Lynch, ‘Hospital anxiety depression scale (HADS) questionnaire predicts response to ketamine infusion therapy in patient with chronic pain’
- 2009: Dr Eoin Casey ‘Bolus Remifentanil for Chest drain removal in the Intensive Care unit: A comparison of two doses versus placebo’ and Dr Tanya O’Neill ‘Post-Operative Cognitive Dysfunction: the contribution f general anaesthetic agents to its aetiology’
- 2008: Dr Dominic Hegarty,
- 2007: Dr Brian Pickering ‘“Anaesthetic agents differentially affect intracellular calcium homeostasis in both resting and stimulated neuronal cells’
- 2006: Dr Michael O’Dwyer ‘The occurrence of severe sepsis is related to distinct patterns of cytokine gene expression’
- 2005: Dr Robert Plant ‘Systemic and myocardial manifestation of the inflammatory response to cardiopulmonary bypass and the heat shock response’
- 2004: Dr Chrisen Maharaj, Effects and mechanism of action of volatile agents on the foetal-placental vasculature”
- 2002: Dr David Honan, “Hypercapnic acidosis may attenuate endotoxin induced acute lung injury by a nitric oxide dependant mechanism”
- 2001: Dr Catherine O’Malley, “The effects of pharmacologic attenuation of haemodynamic responses to experimental aortic cross clamping on the splanchnic circulation”
- 1997 Dr Craig Renfrew, “A new method of Carbon Dioxide absorption for Low-flow Anaesthesia”
- 1994: Prof Donal Buggy, “Posterior column sensory impairment during ambulatory epidural analgesia for labour”
The award was previously named the Abbott Scholarship in Anaesthetic Research. The €10,000 scholarship fund is provided by Abbott Laboratories and is awarded to support original research by an Irish Anaesthetist. In 2013 Abbott was rebranded and renamed Abbvie. Applications are open to non -consultant Anaethetists in Ireland. To apply applicants must complete an application form, submit a short curriculum vitae, full colour passport size photograph and a description and rationale of their research in no more than 1,000 words. All applications are reviewed by three judges. Selected applicants are interviewed and present their proposed research project to a panel of judges. Each presenter is limited to 10 minutes. The award is presented to the winner at the annual Irish Congress of Anaesthetists. The successful applicant is required to produce a progress report to the Education Committee of the College of Anaesthesiologists of Ireland six months after the work has been completed. The winner must send a written report at the completion of the project. Research findings should be submitted for publication in a peer review journal. Applications are open from January and presentations are held in March annually. The competition is advertised by the Education Department (CAI) , application information is available on the College website (www.anaesthesia.ie). The scholarship is advertised to all trainees who are contacted directly application information is also distributed around all training hospitals.
Winners
- 2024: for 1st Dr Clodagh Staunton Curren – Implementing a ‘Sip til Send’ policy at a large tertiary referral centre; 2nd 100% refer organ donation model in St James Hospital. Dr Fionn Clarke; 3rd “Get with it” ward based management of total abdominal hysterectomy patients receiving intrathecal morphine. Dr Darragh McKeon.
- 2021: Dr Rachel Nolan, ‘Improving Discharge Prescribing in a Tertiary Referral Centre’
- 2018: Dr Moninne Creaney, ‘Neuraxial antisepsis in obstetric units – what is the safest option? An audit of national practice.
- 2017: Dr Ciara Hayden, ‘Perioperative glycaemic control and its association with post-operative infection in patients undergoing cardiac surgery on cardiopulmonary-bypass (CPB)
- 2016: Dr Gareth Morrisson, ‘Improving airway safety within the Intensive Care Unit – a new course to ”SCREAM” about’
- 2015: Drs Colm Keane, ‘Cell therapies for Sepsis’ and Dr Kirk Levins, Effect of anaesthetic technique on immune cell infiltration in breast cancer: A prospective, ramdomised, investigator – masked study’
- 2014: Dr Anne Doherty ‘Apelin, Placental Growth Factor and Soluble fms-like tyrosine kinase-1 at 14-16 weeks gestation in Pregnancies Complicated by early Preeclampsia and/or Fetal Growth Restriction.’
- 2013: Dr Caroline Larkin ‘The Mechanisms of sepsis-associated thrombocytopenia and thrombosis’ and Dr Noelle Murphy ‘The Validation of urinary biomarkers of acute kidkney injury (AKI) post open aortic abdominal aneurysm repair’
- 2012: Dr Noelle Murphy ‘The role of gremlin in the evolution of the acute respiratory distress syndrome’ and Dr Grace Donnelly ‘What is minimum training required for anaesthetists to be able to perform rigid bronchoscopy? A study in manikins’
- 2011: Dr Robert Grealy for his presentation entitled ‘Transcriptomic Profiling of Monocytes in Sepsis’
- 2010: Dr Stephen Frohlich “Signaling Pathways that Protect against lung damage in the acute respiratorydistress syndrome: Creb Responsive Genes in the Lung” and Dr Mairead Hayes “Determination of the potential for mesenchymal stem cells to reduce injury and enhance repair following sepsis induced Acute Lung Injury”.
- 2009: Dr Ivan Hayes ‘“Intralipid in Asphyxial Cardiac Arrest- A Laboratory Study’ & Dr Criona Walsh ‘Volatile Anaesthetics nd Cardioprotectinon: The Role of Redox – Sensitive Inducible Modulators of Mitochondrial Energetics’
- 2008: Dr Tanya O’Neill ‘Post – Operative Cognitive Dysfunction: The Contribution of General Anaesthetic Agents to its Aetiology and the Role cognition enhancing drug therapies in mitigating its development’
- 2007: Dr Roger McMorrow and Dr Pádraig Mahon
- 2006: Dr Martin Duffy ‘Modulation of endothelial dysfunction in the development of sepsis-induced acute long njury by hydroxyl-methyl coenzyme areductase in inhibition with simvastatin’
- 2004/2005: Dr Alistair Nichol ‘Characterization of the molecular mechanisms underlying the protective effects of Hypercapnic Acidosis in Acute Lung Injury’
The Faculty of Pain Medicine was formally inaugurated at a ceremony in the Royal College of Physicians of Ireland November 22nd 2008. It had existed in shadow form for the previous year. The Faculty is a natural progression from the Pain Medicine Board within the College chaired by Dr John Cooper which was set up in 1999. This Board had successfully established the Diploma in Pain Medicine as the first post graduate examination in Europe (2001-2012). The remit of the Faculty is training, education and standards in Pain Medicine in Ireland. Currently admission to the Faculty Fellowship is by examination (Diploma in Pain Management) and following this, passing Part 2 of the fellowship examination. The Fellowship in Pain Medicine, FFPMCAI, was established in 2013. The Diploma in Pain Medicine Medal is awarded to a candidate who achieves A grades in each component of the examination on their first sitting of the exam.
Recipients
- 2021 – Cillian Suiter
- 2013 – Christine Cleary
- 2011 – Fiona Desmond
The inaugural competition for the Clinical Research Medal in Pain Medicine was held in January 2016. The Medal competition is judged by the RYND lecturer of that year. This will be an annual competition which is open to doctors training in pain medicine who have not yet been appointed to substantive consultant posts.
Clinical Research Medal 2021:
- Presenter: Dr Sinead Forde
Clinical Research Medal 2020:
- Presenter: Dr Amy Donnelly
Clinical Research Medal 2019:
- Presenter: Deborah Galvin
Clinical Research Medal 2018:
- Title: A Retrospective Audit of Pulsed Radiofrequency Adjacent the Cervical Dorsal Root Ganglion.
- Presenter: Aine O’Gara.
Clinical Research Medal 2017:
- Title: Characterisation of Central Neuroimmune Response following thoracotomy and the development of neuropathic pain.
- Presenter: Jonathan Royds
The Inaugural Francis Rynd Lecture took place on the 16 February 2012 in the College of Anaesthesiologists, Merrion Square and the Rynd Lecture is now a central component of the Annual Scientific Meeting of the Faculty of Pain Medicine. Dr Francis Rynd was a surgeon at the Meath Hospital, who developed the first device to deliver medication by injection in 1844. Later his concept was adapted to become the modern hypodermic syringe. Furthermore the patient who received the first injection of morphine creosote was suffering from intractable facial pain and was in essence the first patient suffering from chronic pain anywhere to receive an interventional pain procedure to relieve their pain. The importance of this contribution to modern medicine is captured by the Chief Herald in the coat of arms awarded to the Faculty of Pain Medicine –the cross like structure which looks like a surgical instrument is from the Rynd family crest.
- 2024: Dr Siobháin O’Mahony
- Francis Rynd Lecture 2021, Title: Imaging Pain, Analgesia and Anaesthesia induced Altered States of Consciousness Presenter: Prof Irene Tracey, Warden, Merton College, Professor Anaesthetic Neuroscience, Nuffield Department Clinical Neurosciences & Pro-Vice Chancellor, University of Oxford, England UK
- Francis Rynd Lecture 2018, Title: Phenotyping the pain patient: preparing for the advent of precision medicine Presenter: Professor Ralf Baron, Head of the Division of Neurological Pain Research and Therapy and Vice Chair of the Department of Neurology, Christian-Albrechts-Universitaet Kiel, Germany.
- Recent Lectures Francis Rynd Lecture 2017, Title: Heterogeneity in neuropathic pain Presenter: Professor Andrew Rice, Professor in Pain Research, Imperial College, London.
Thomas James Gilmartin, 1905-1986. First Dean of the Faculty of Anaesthetists, RCSI. Thomas Gilmartin was born in Ballymote Co. Sligo in 1905 and educated at Summerhill College and subsequently Belvedere College Dublin. He attended medical school at the Royal College of Surgeons in ireland and graduated L.R.C.P.S.I in 1929. He then trained in Anaesthetics in Liverpool and London.He was appointed assistant anaesthetist in Mercers Hospital in 1932 and full consultant in 1946. He is credited with introducing Thiopentone to anaesthetic practise in Ireland in 1934 and subsequently curare in 1945. He was involved in development of the first Diploma in Anaesthetics which was a conjoint examination of both the Royal College of Physicians and Surgeons of Ireland, which was held for the first time in 1942 and which he received in 1943. In 1945 he applied to the Royal Academy of Medicine in Ireland to form a section of Anaesthetics. Permission was granted provided a committee of 12 be formed. The committe was created with TPC Kirkpatrick as President and Tommy Gilmartin as secretary. At their inaugral meeting Sir Ivan Magill spoke on “Current topics in anaesthetics.” He subsequently held the role of president of the anaesthetic section RAMI. In 1949 he was a foundation fellow of the new Faculty of Anaesthetists of the Royal College of Surgeons (England) In 1959 he was a founding member and first dean of the Faculty of Anaesthetists of the Royal College of Surgeons in Ireland. He was also a founding member of the Association of Anaesthetists of Great Britain and Ireland (AAGBI) in 1932, was a council member and vice-president(1973-1975). He was awarded the John Snow Medal by the AAGBI in 1985. He was made an Associate Professor of Anaesthetics by the RCSI in 1965, the first academic post in the Republic of Ireland , just a year after the appointment of John Dundee as Professor in Belfast. He received an Honorary F.R.C.S.I. in 1974.The Gilmartin lecture was inaugurated in his honor following his death in 1986.
Gilmartin Lecture Speakers
- 2023: Prof Mary Horgan
- 2021: Mr Turtle Bunbary,‘ Of Chloroform, Contagion & the Comanche Nation: Aspects of the World in 1847’
- 2020: Dr Miram Colleran, ‘The palliative care in ICU in a time of change’.
- 2019: Dr Brendan Rooney, Head Curator at National Gallery of Ireland, ‘Irish by definition. Hanging a National Collection’.
- 2018: Prof Brendan Kelly, Professor at Psychiatry at Trinity College Dublin and Consultant Psychiatrist at Tallaght University Hospital, ‘How To Be Happy’.
- 2017: Dr Barbara Dawson, Director of Dublin City Gallery The Hugh Lane, ‘Who needs art’.
- 2016: Prof Deborah Kelleher, Director of the Royal Irish Academy of Music (RIAM). ‘Spackling Band: What can we learn from the music of Georgian Dublin?’
- 2015: Dr Joe Tracey, Retired Consultant Anaesthetist, ‘250 years at 22 Merrion Square’. The story of the house and the specialty’
- 2014: Dr Rhona Mahony, Master of National Maternity Hospital Holles St, Dublin. ‘Take Me Away From The Monto’
- 2013: Professor Aidan Halligan, Director of Education at University College London Hospitals. ‘Rediscovering Lost Values’.
- December 2012: Mr Kevin O’Sullivan, Editor of the Irish Times Newspaper. “Why Quality Newspapersmatter in the Ireland of 2012”
- May 2012: Mrs Margaret Murphy, Expert Lead, Patients for Patient Safety, World Health Organization. ‘The Patient Experience as a Catalyst for Change’
- 2011: Prof Charles Normand, Edward Kennedy Prof of Health Policy and Management, Trinity College Dublin. “Doing more for less”
- 2010: Mr Marc Coleman, Economic Editor of Newstalk Radio Station
- 2009: Prof Paul Muldoon, Professor of English, Princeton University
- 2008: Dr Archie Brain ‘LMA’
- 2007: Prof Garret Fitzgerald ‘NSAIDS and Beyond: Cardiovascular Consequences of COX inhibition’
- 2006: Dr John Hillery ‘Professional Self Regulation in the 21st Century: Hall-mark or outdated artefact?’
- 2005: Prof Carol Black ‘The changing practice of Medicine’
- 2004: Prof Richard M Satava, Professor of Surgery University of Washington, USA, ‘The Bio intelligence age –Science & Healthcare after the information age’
- 2003: Mr Michael McDowell, Minister for Justice
- 2001: Micheal Martin, Minister for Health & Children
- 1997: Art Cosgrove, President UCD, ‘The Universities Bill 1996’
KP Moore Medal This competition is organized by the Committee of Anaesthetists in Training (CAT) and is aimed at trainees in their first few years of training. The competition was previously named the GSK Medal Competition but was renamed in 2012 in honour of Dr Kevin P. Moore. To be considered for presentation at the KP Moore Medal Competition, applicants must submit an abstract of their work based on clinical cases related to Anaesthesia, Intensive Care or Pain Management. Six abstracts are shortlisted by three judges who then assess the full text of these application. There is a time limit of ten minutes for each presentation in the competition and the judges may then ask questions for a further 5 minutes. The competition is held annually. Applications are open from September and presentations are in November at the Winter Anaesthesia College Weekend. The competition is advertised by the Education Department (CAI), application information is available on the College website (www.anaesthesia.ie); all trainees are contacted directly and application information is distributed around all training hospitals. The winner of the competition is announced that evening and is awarded the KP Moore Medal. Kevin P Moore MB BCh BAO, FFARCS, FFARCSI (1936 – 1997) Kevin Patrick Moore was born 1936. He was educated at Belvedere College and attended Medical School at University College Dublin (UCD) and graduated MB, BCh BAO in 1960. Having completed his intern year at the Mater Misericordiae Hospital, Dublin, Dr. Moore began training in anaesthesia in the UK where he worked at the Leeds General Infirmary and the Queen Elizabeth Hospital, Birmingham. He returned to Ireland in 1970 to take up the post of consultant paediatric anaesthetist at Our Lady’s Hospital for Sick Children, Crumlin. The Hospital had been opened in 1956 but Dr Moore was only the second full time consultant anaesthetist to be appointed at Our Lady’s. Over the following decades the development of paediatric anaesthesia at Our Lady’s Hospital and of training in anaesthesia in general, were closely linked, and Kevin Moore was at the heart of both. The Eastern Regional Anaesthetic Training Scheme was established in 1972 and the National Senior Registrar Training Scheme followed shortly afterwards in 1976. Both training schemes were administered and run by the Medical Advisory Committee of the Faculty of Anaesthetists RCSI which was chaired by Dr. Moore for many years. Dr. Moore also served as an elected member of the Board of the Faculty of Anaesthetists RCSI (1982 – 1992) and as Vice Dean (1991 – 1992). A gifted clinician and paediatric anaesthetist, Kevin Moore was also revered as a teacher, an administrator, for his wit, his kindness and his indomitable spirit. During a career spanning more than 25 years at Our Lady’s, Kevin Moore inspired numerous anaesthetic trainees and helped to equip them with a knowledge and appreciation of paediatric anaesthesia which has remained a corner stone of their own careers as consultants in Ireland and abroad.
K P Moore Medal Winners Presentation Title (GSK Medal prior to 2012)
- 2024: Dr Ben Atterton from Letterkenny General Hospital and the Poster prize was won by Dr Ahmed Hassan Mohi Eldeen Mohammed form Our Lady of Lords Hospital Drogheda
- 2021: Dr Mai O’Sullivan, ‘Simulating high-fidelity emergency front-of-neck access training in an obstetric setting’
- 2020: Dr Michael Ma, ‘Anaesthetic Education in Medication Safety – The Use of Simulation Debrief to Improve Standards of Care’
- 2019: Dr Robert Owens, ‘Medication Safety in Anaesthesia; A Novel Approach to Improving Standards of Care’
- 2018: Dr John O’Shea, ‘The Evaluation of an Online Preoperative Assessment Tool’
- 2017: Dr Martina Melvin, ‘ Neuro-T , a Smartphone App to aid in the safe transfer of the Emergency Neurosurgical Patient to Beaumont Hospital’
- 2016: Dr Joao Marques Vinagre, ‘Pulsed radiofrequency of the brachial plexus in the treatment of post-radiotherapy neuropathic upper limb pain’
- 2015: Dr Georgina Duignan, ‘A Tale of Two Fishermen
- 2014: Dr Pierce Geoghegan, ‘Sodium correction practice in profound hyponatremia: experience in a tertiary referral centre’
- 2013: Dr David Moore, ‘Use of a multi-modal care pathway for laparoscopic cholecystectomy’
- 2012: Dr Ghulam Raza, ‘Use of the Airway Exchange Catheter technique for ‘at-risk’ extubation: a case report’
- 2011: Dr Noelle Murphy, ‘Recognition of ARDS/ALI at the Bedside and clinic-pathological correlation’
- 2010: Dr Kingsley Enohumah’ Acquisition of intubation skill with difficult airway devices. A comparison of Airtraq and Levitan scopes in a Manikin’
- 2009: Dr Alexandra Crean ‘Severe rhabdomyolysis due to a drug interaction’
- 2008: Dr Niamh McAuliffe “The Long Road to Diagnosis: A Case of Neuromuscular Weakness in ICU’
- 2007: Dr Catherine Nix ‘Does unintentional dural puncture predispose to postpartum cerebral venous sinus thrombosis? Two case reports’
- 2006: Dr Amer Iqbal Jaura ‘ The Management of Acute Tracheooesophageal Tear in a Polytrauma Patient by Bilateral Endobronchial Intubation’
- 2005: Dr Grainne McDermott ‘Anaesthesia for caesarean section in a case of Spina Bifida and Pierre-Robin sequence’
- 2004: Dr Eoin Casey ‘Survival Rate Following Admission to ICU Post Cardio – Pulmonary Arrest; Mater Figures 2003’
The Joint Faculty of Intensive Care Medicine of Ireland is the body in Ireland responsible for higher professional training in Intensive Care Medicine in Ireland. It took over the role of the Irish Board of Intensive Care Medicine in 2009 and is a Joint Faculty, in that it has representation of all the post-graduate training bodies – the College of Anaesthesiologists of Ireland, the Royal College of Surgeons in Ireland, and the Royal College of Physicians in Ireland, as well as representation from the Intensive Care Society of Ireland. This medal is awarded for outstanding achievement in this exam.
Recipients
- 2024 – Dr Ciaran Costello
- 2020 – Andrew Neill
- 2019 – Pierce Geoghegan
- 2018 – Sean Keane
- 2017 – No winner
- 2016 – No winner
- 2015 – Mary Aisling McMahon
- 2014 – Maeve Henry
- 2014 – Kate O’Donnell
- 2013 – No winner
- 2012 – No winner
Diploma in Intensive Care Medicine Medal Award
- 2011 – Jennifer Hastings
- 2010 – David Hendron
- 2009 – Caitriona Murphy
- 2006 – Donal Ryan
- 1999 – Arabella Fahy
This lecture is held in conjunction with the KP Moore Medal Presentations (previously the GSK Competition) and in recent years as part of the Winter Anaesthesia Weekend. The presenter of this prestigious event is awarded the Winter College Lecture Medal by the College.
Previous Winners
- 2024: Prof Jeffery Cooper
- 2021: Martin Bromiley OBE, Airline Captain & Founder, The Clinical Human Factors Group, ‘The thin line between success and failure and how you can stay on the right side of it’
- 2020: Dr Michael J Ryan, Executive Director WHO Health Emergencies Programme, ‘COVID-19: Fighting smart & safe in the front-lines of an emergency’
- 2019: Prof Ravi Mahajan, President of Royal College of Anaesthetists, UK, ‘Perioperative Medicine and Patient Safety’.
- 2018: Mr Jim Gavin, Assistant Director at Irish Aviation Authority, ‘Leadership: A Contact Sport’.
- 2017: Dr Jannicke Mellin-Olsen, President Elect, World Federation of Societies of Anesthesiologists ‘Helsinki Declaration on Patient Safety I Anesthesiologists What is next in Europe and the World?’
- 2016: Dr Brian Marsh, Consultant in Anaesthesia & Intensive Care Medicine Clinical Director – CCAEST, Mater Hospital. ‘How shall we care for our elderly critically ill’
- 2015: Dr John Carlisle, Intensivist, Torbay hospital, Devon, UK. ‘Most research findings are false, occasionally because researchers make stuff up’.
- 2014: Prof Paul Myles, Director, Dept of Anaesthesia and Perioperative Medicine, Alfred Hospital and Monash University, Melbourne, Australia.
- 2013: Prof Justiaan Swanevelder, Professor and Head of Department of Anaesthesia at the University of Cape Town, Groote Schuur and Red Cross War Memorial Children’s Hospitals in South Africa. ‘The value of Perioperative Echocardiography’ ‘The safety of nitrous oxide: the findings of the ENIGMA-II trial’.
- 2012: Dr William Harrop-Griffiths ‘Innovation, Technology and Safety A sceptic’s view of a changing world’.
- 2011: Dr David Bogod, President of the Obstetric Association of Anaesthetists, is entitled “Medicolegal implications of nerve blocks and neuraxial anaesthesia”.
- 2010: Dr Donal Nyhan, “Vascular Biology of Ageing”
- 2009: Prof Scott Beattie ‘A Framework for Making Evidence Based Decisions in Anaesthesia’
- 2008: Dr Jennifer Hunter ‘A Novel Approach to Reversal’
- 2007: Prof Beverley Orser ‘MAC, Memory and the Mechanisms of Anaesthesia’.
- 2006: Prof Mark Warner ‘“Perioperative Neuropathies, Blindness and Positioning Problems’.
- 2005: Dr Monty Mythen ‘Are your gases flowing freely?”
- 2004: Dr Brian Kavanagh ‘Research in Anaesthesia: The Future and The Need’
College of Anaesthesiologists of Ireland Final FCAI Medal The Final FCAI Medal is awarded at the annual conferring ceremony in May. The prize is awarded to a candidate who achieves first place at both the Spring and Autumn iterations of the Final examination. This Medal was donated by Professor Tess Cramond (Brophy) AO OBE FRCA FANZCA, Hon FFARCSI, FFP MANZCA, in memory of her parents William and Jane Brophy (nee O’Rourke). All four of Professor Cramond’s grandparents were Irish. They migrated to Australia in the late 1870s and settled in Queensland. Like so many of the Irish in Australia, they gave to their children, including their daughters, the benefits of secondary education when this was a privilege afforded few women. William and Jane Brophy continued this tradition and supported education, not only of their four daughters, but also by supporting education for the trades and for the development of like skills, particular for those not aspiring to tertiary education. While maintaining a love of Ireland and its history and traditions, Professor Cramond’s grandparents and parents espoused the philosophy of being ‘faithful to the Old Land, true unto the New’. It is for this reason that she has donated The William and Jane Brophy Prize as witness to the links between Ireland and Australia. Tess Cramond graduated from the University of Queensland in 1951, and undertook intern, resident and initial registrar training at the then Brisbane Hospital before proceeding to the United Kingdom where she obtained FFARCS. On return to Australia three years later, she was not only admitted FFARACS, but also embraced enthusiastically a commitment to teaching and training of medical students, registrars and health professionals in anaesthetics, resuscitation, palliative medicine and pain medicine. She was appointed Foundation Professor of Anaesthetics, University of Queensland in 1978, but made time as well to contribute to the administrative side of a young specialty, especially the Faculty of Anaesthetists as Examiner and Dean, as Examiner in Pain Medicine, the Australian Medical Association, the Australian Society of Anaesthetists, and as a Colonel in the Royal Australian Army Medical Corps Reserve. Her major community service has been through Surf Life Saving Australia as Chairman of its Medical Advisory Committee for 30 years. In 2011 Professor Cramond was the guest lecturer at the annual scientific meeting of the Faculty of Pain Medicine and was made an Honorary Fellow of the Faculty of Pain Medicine, College of Anaesthesiologists of Ireland. Professor Cramond passed away in 2016 but will be fondly remembered as a pioneer of Australian anaesthesia and pain medicine and a great friend of the College and Faculty in Ireland.
Previous Medal Winners
- Spring 2024 – Dr Brian Doyle
- August 2023 – Dr Aoife Brady
- Spring 2021 – Robert Owens
- Autumn 2020 – Daniel Mulligan
- Autumn 2019 – Syed Ziad Ali
- Autumn 2019 – Stephen Murphy
- Spring 2019 – David Burke
- Autumn 2018 – Johnathan Roddy
- Spring 2018 – Robert Ffrench O’Carroll
- Spring 2018 – Shane O’Sullivan
- Autumn 2017 – Niamh Barnwell
- Spring 2017 – Paul Fennessy
- Autumn 2016 – Pierce Geoghegan
- Spring 2016 – Muhammad Kashif
- Autumn 2015 – Laura Flood
- Spring 2015 – Aidan Magee
- Spring 2015 – Ursula McHugh
- Autumn 2014 – Mary Aisling McMahon
- Autumn 2014 – David Greaney
- Aoife Hegarty – Spring 2013
- Ahmed Elsherbeny – Spring 2013
- Raymund O’Connor – Spring 2012
- Roseita Caroll – Spring 2012
- Karen Goddard – Spring 2011
- Aine Heaney – Spring 2011
- Niall Kennedy – Spring 2011
- Fiona Kiernan – Autumn 2010
- Michael Callaghan – Spring 2008
- Payal Kajekar – Spring 2008
- Denise McCarthy – Spring 2007
- Mark Dougherty – Spring 2006
- Michael Looney – Spring 2006
- Róisín Ní Mhuircheartaigh – Autumn 2004
- Aoibhin Hutchinson – Spring 2004
- Raymond McKee – Spring 2004
- Donal Ryan – Autumn 2003 Nilesh Nanavati – Spring 2003
- Gareth Allen – Spring 2002
- Raman Sivasankar – Spring 2002
- Mark Nash – Autumn 2001
- Bronagh McElhenny – Autumn 2001
- Adam Harper – Spring 2001
- Ruth Fanning – Autumn 1999
- Clive Woolfe – Autumn 1995
- Donal Buggy -Spring 1995
- Abhiram Mallick – Autumn 1994
- Catherine Angela O’Dwyer – Spring 1993
- Joseph Francis Fitzgerald – Autumn 1993
- Willie O’Brien – Autumn 1975
Recent Winners:
- 2024: Dr Gareth Morrison
- 2023 Colm Bergin
- 2022 John Cahill
- 2022 Joe Tracey
- 2022 Declan Ward
Winners
- 2024: Dr Siobhain M O’Mahony
- 2023 – Margaret Murphy
- 2023 – Mohammad Shoaib Shafi
Recipients
- 2024 – Dr Jenny Fitzgibbon